Whiplash, or WAD (Whiplash Associated Disorders), refers to a neck injury where the normal range of motion is exceeded, resulting in injury to the soft-tissues (hopefully with no fractures) in the cervical region. There are a LOT of factors involved that enter into the degree of injury and length of healing time. Let’s take a closer look!
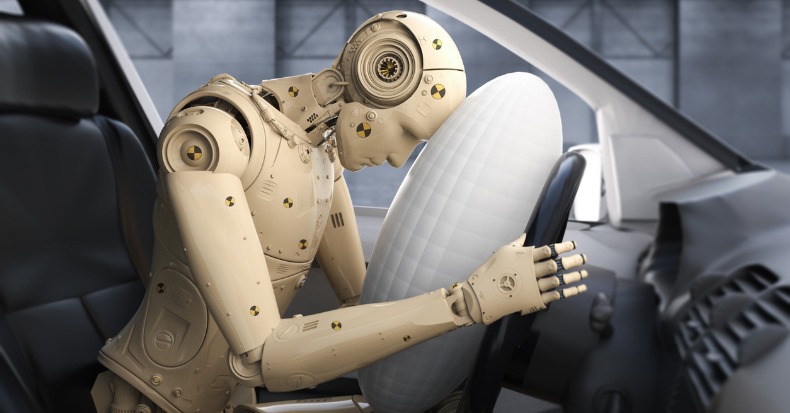
Picture the classic rear-end collision. The incident itself may be over within 300 milliseconds (msec), which is why it’s virtually impossible to brace yourself effectively for the crash as a typical voluntary muscle contraction takes two to three times longer (800-1000 msec) to accomplish.
In the first 50 msec, the force of the rear-end collision pushes the vehicle (and the torso of the body) forwards leaving the head behind so the cervical spine straightens out from its normal “C-shape” (or lordosis). By 75-100 msec, the lower part of the neck extends or becomes more C-shaped while the upper half flexes or moves in an opposite direction creating an “S” shape to the neck. Between 150-200msec, the whole neck hyper extends and the head may hit the head rest IF the headrest is positioned properly. In the last 200-300 msec, the head is propelled forwards into flexion in a “crack the whip” type of motion.
Injury to the neck may occur at various stages of this very fast process, and many factors determine the degree of injury such as a smaller car being hit by a larger car, the impact direction, the position of the head upon impact (worse if turned), if the neck is tall and slender vs. short and muscular, the angle and “springiness” of the seat back and relative position of the headrest, dry vs. wet/slippery pavement, and airbag deployment, just to name a few.
Some other factors that can predict recovery include: limited neck motion, the presence of neurological loss (nerve specific muscle weakness and/or numbness/tingling), high initial pain levels (>5/10 on a 0-10 scale), high disability scores on questionnaires, overly fearful of harming oneself with usual activity and/or work, depressive symptoms, post-traumatic stress, poor coping skills, headaches, back pain, widespread or whole body pain, dizziness, negative expectation of recovery, pending litigation, catastrophizing, age (older is worse), and poor pre-collision health (both mental and physical).
Research shows the best outcomes occur when patients are assured that most people fully recover and when patients stay active and working as much as possible. Studies have shown it's best to avoid prolonged inactivity and cervical collars unless under a doctor's orders. It's also a good idea to gradually introduce exercises aimed at improving range of motion, postural endurance, and motor control provided doing so keeps the patient within reasonable pain boundaries. Chiropractic manipulation restores movement in fixed or stuck joints in the back and neck and has been found to help significantly with neck pain and headaches, particularly for patients involved in motor vehicle collisions. A doctor of chiropractic may also recommend using a cervical pillow, home traction, massage, and other therapies as part of the recovery process.
It is important to be aware that fear of normal activity and not engaging in usual activities and work can delay healing and promote chronic problems and long-term disability. It's suggested patients avoid opioid medication use due to the addictive problems with such drugs. Ice and anti-inflammatory herbs or nutrients (like ginger, turmeric, and bioflavonoids) are safer options. Your doctor of chiropractic can guide you in this process!